Varicose Veins – Everything You Need To Know

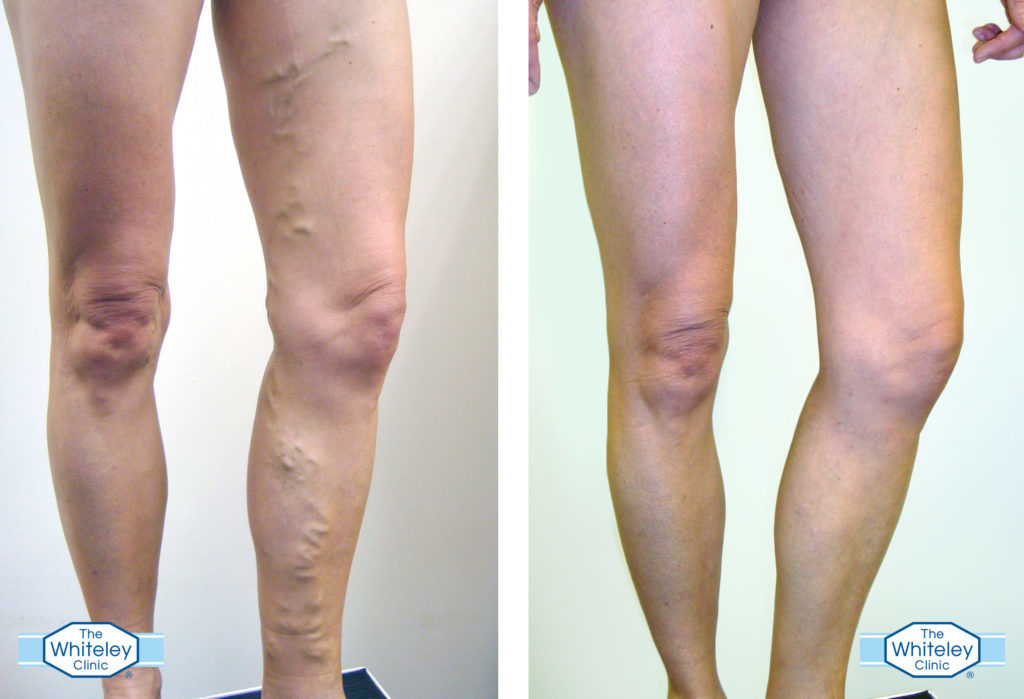
Varicose veins are a condition that will affect up to 30% of us in our lifetime. Most of us are familiar with these unsightly, knobbly red and blue lumps on the legs, yet there is still an awful lot of confusion surrounding what they are and where they come from.
Here, leading vascular specialist Professor Mark Whiteley of The Whiteley Clinic, shares his expert knowledge about the condition:
What Are Varicose Veins?
Professor Whiteley says: “Varicose veins occur when valves in our leg veins stop working properly, meaning the blood falls down the veins when standing up, rather than flowing upwards towards the heart. In their simplest form, varicose veins can be identified as bulging veins which protrude from the legs, however, shockingly up to half of all varicose veins sufferers will show no overt signs of the condition, as the problematic veins remain hidden under the skin.”
What Are The Causes Of Varicose Veins?
Professor Whiteley says: “There is a stereotype that it is only the old and the overweight who will suffer from varicose veins. The truth is, 30% of all adults will be affected by them and contrary to popular belief; the condition is familial and can strike at any time of life – although it does become more common with passing years. This said, that doesn’t stop young people getting them if their genes determine it. I recently operated on a 12-year-old boy with severe varicose veins and have had many other patients in their teens.
“Up to 89% of people who believe they are suffering from harmless thread veins on the surface of their skin are actually displaying signs of these hidden varicose veins. Many people will ignore these veins as they assume they are purely a ‘cosmetic condition’, and will often seek simple removal of these thread or spider veins. However, if the underlying hidden varicose veins have not been found and treated first, then thread or spider vein treatments are much less likely to work. Indeed, failure to find and treat the underlying veins can result in permanent red stains in a few cases.”
When Is The Best Time To Treat Varicose Veins?
Professor Whiteley says: “Many people will feel self-conscious about baring their legs during the summer months because of varicose veins, especially as 50% of varicose veins are visible with a bulging appearance. It is very common for patients to seek treatment later in the year when their summer holidays are looming, but unfortunately this does not allow enough time for the course of the treatment to complete – which is why January and February are the perfect time to start!”
How Are Varicose Veins Treated?
Professor Whiteley says: “There are a number of cutting-edge endovenous techniques available for treating varicose veins both quickly and effectively – we have come a long way since the outdated technique of stripping! Cutting-edge techniques which we use today at The Whiteley Clinic include:
- EVLA (ENDOVENOUS LASER ABLATION): This technique destroys the veins at the root of the problem, under local anaesthetic, as a walk in, walk out procedure.
Under ultrasound control, a needle is placed in the vein near the knee or ankle. A wire is then passed into the vein and a long “sheath” is passed up the vein to the top. The ultrasound is used to position the end of the sheath exactly.
Local anaesthetic is injected around the vein – again using ultrasound to make absolutely sure the fluid is in the right place.
Once the anaesthetic is in place, the laser fibre is passed up inside the sheath until it comes out of the top. The fibre is fixed to the sheath and the laser is switched on. The sheath and laser are then pulled back at an exact rate, making sure the vein is completely destroyed – but without damaging the surrounding tissues.
- VENASEAL: The Venaseal or “superglue” treatment is a relatively new way of closing the main vein in the leg that causes varicose veins. When Venaseal is performed, only one needle hole is needed per vein treated so there is no need for the additional injections of local anaesthetic around the vein – unlike endovenous laser ablation or radiofrequency ablation.
Not every patient is suitable for the Venaseal treatment so it’s important that a duplex ultrasound scan is carried out to assess suitability.
- FOAM SCLEROTHERAPY: Ultrasound guided foam sclerotherapy is a highly effective technique to treat small varicose veins.
When the vein is destroyed using sclerotherapy, the liquid kills the cells in the vein wall causing inflammation. When inflamed, the vein becomes hard to the touch. Over a period of several months the body eats away the dead vein, leaving only a tiny bit of scar tissue behind. However, sclerotherapy only works in small veins and if there is no blood in the vein.
- PELVIC VEIN EMBOLIZATION: This is an X-ray technique where a needle is put into a vein and, under X-ray control, a thin tube called a catheter is pushed into the vein we wish to treat. Almost all of our patients with Pelvic Vein Reflux which cause the following, will need treatment – Pelvic congestion syndrome, Vulval varicose veins, vaginal varicose veins, leg varicose veins arising from the pelvis.
Unfortunately, many health professionals are unaware of the existence of these newer, more effective treatments and how to use them to their best advantage, which is why it is always really important to go and see a veins specialist who deals with venous conditions day in day out.”
For more information, visit www.thewhiteleyclinic.co.uk